Last Updated: 07/18/2025
In This Article
What is Mpox (formerly Monkeypox)?
Mpox is a viral disease from the same family as smallpox. It typically presents with a rash along with other symptoms and is usually not life-threatening.
It’s regularly found in Central and West Africa in rodents, monkeys, and other animals with possible animal-to-human transmission. It was first identified in monkeys in 1958, and the first human case was confirmed in 1970.
Is Mpox (Monkeypox) only in Africa?
There are two types of Mpox: Clade I and Clade II. Both of them are endemic to Africa.
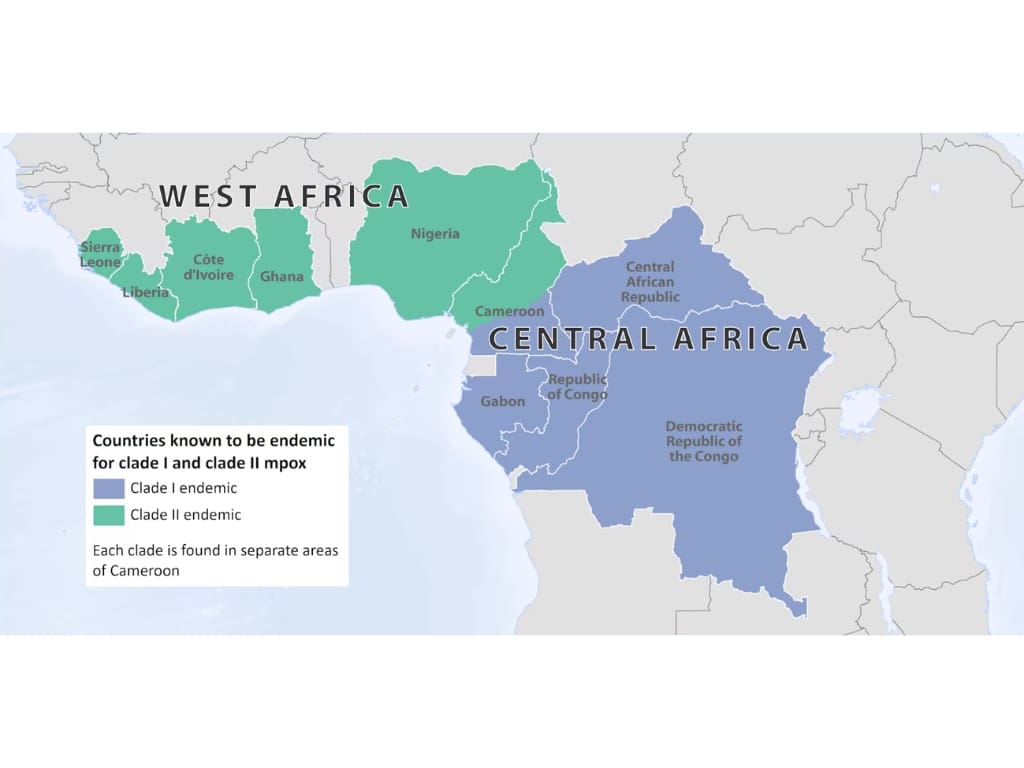
Clade I Mpox
has not been reported in the US. There are just single digits of cases outside of Africa.
This type is causing most cases of current outbreaks in the Democratic Republic of the Congo (DRC) and neighboring countries.
It’s much more deadly, based on the data we have, with a death rate of up to 10% and about 1% – 3.3% in the current outbreak.
Since January 2024, nearly 36,000 suspected cases of Mpox have been reported in the DRC, with a majority being Clade I. However, due to limited diagnostic capacity, only around 7500 of these were confirmed in a lab.
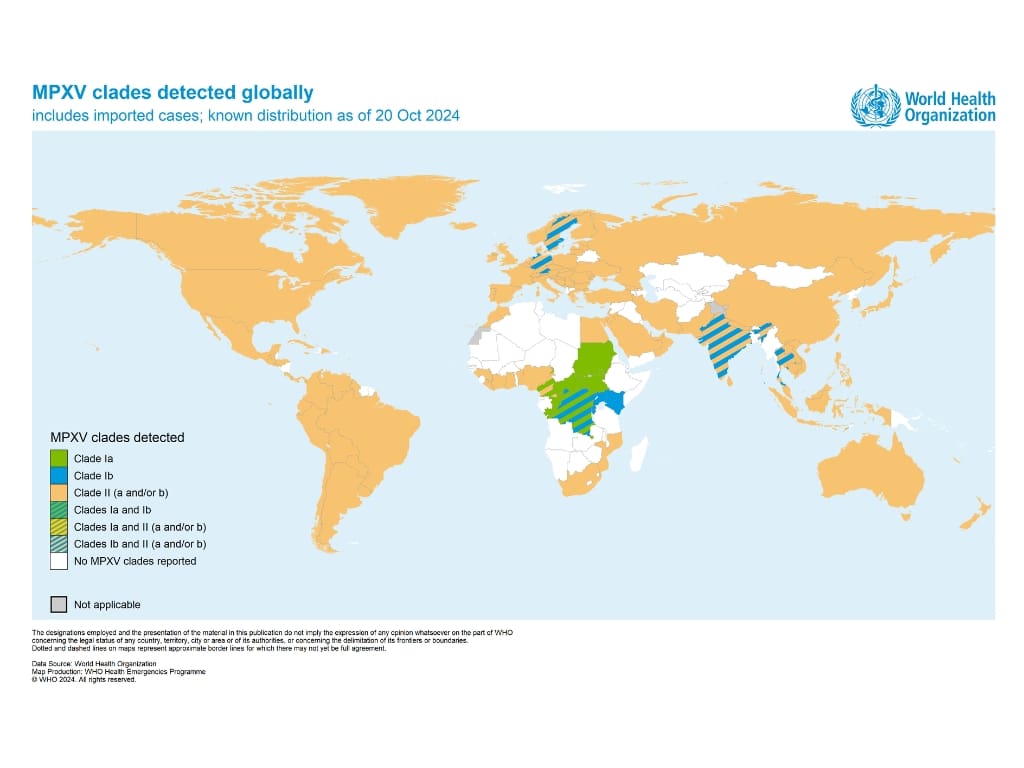
Clade II Mpox
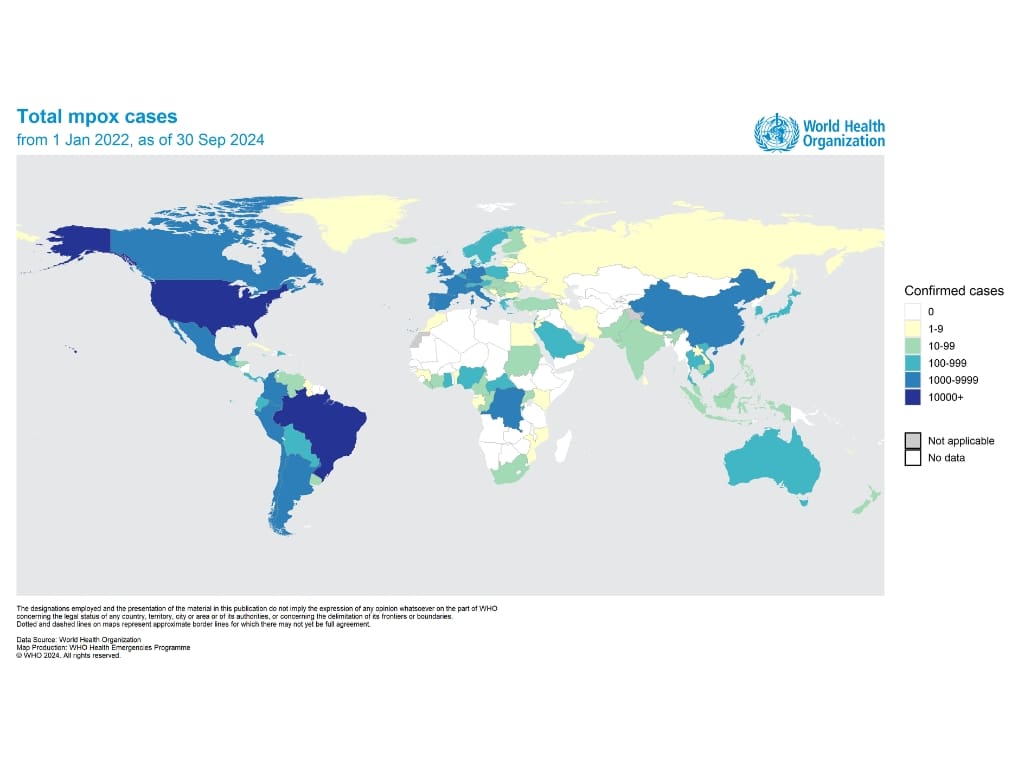
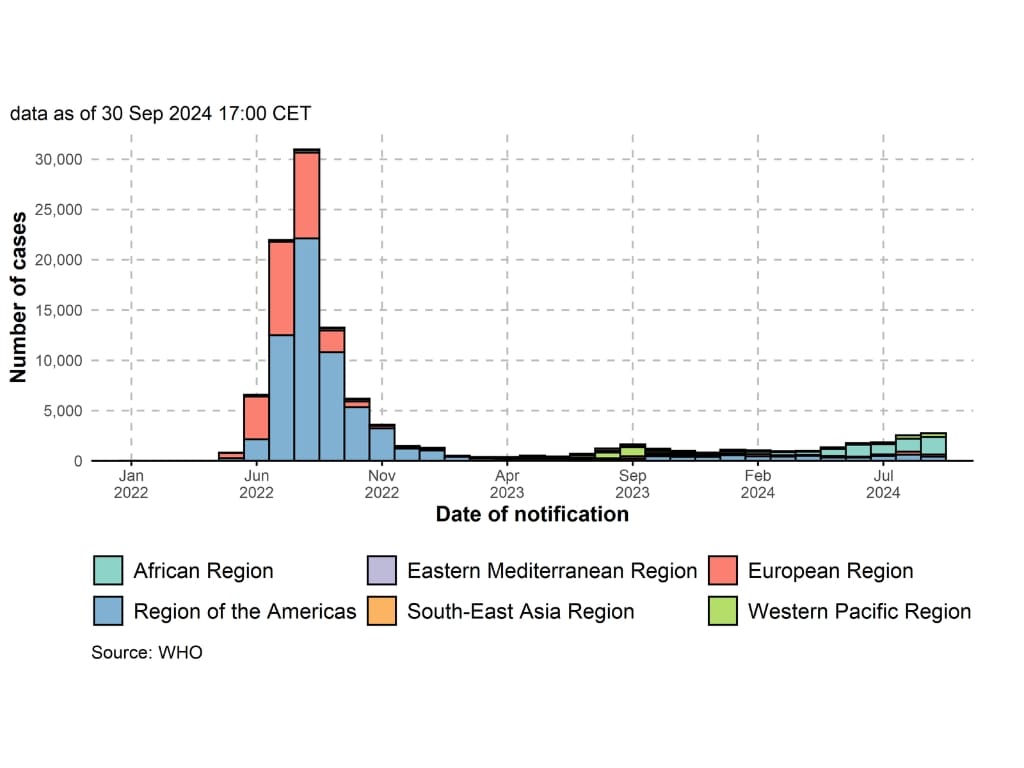
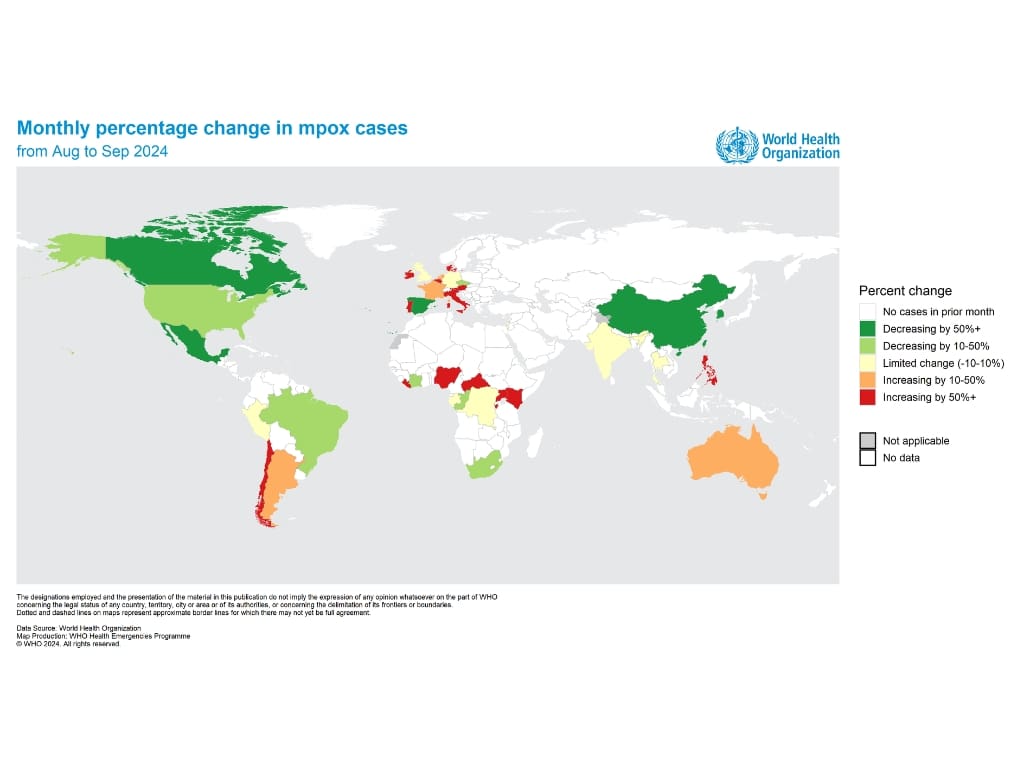
is endemic in Western Africa; however, since the 2022 outbreak, it spread to many countries worldwide, with the majority of confirmed cases in Europe and North America.
Since January 1, 2022, more than 109,000 Clade II cases have been confirmed worldwide, including 236 deaths. The numbers have been decreasing since the 2022 peak. The survival rate is more than 99.9%.
The top three most affected countries by Mpox are the USA, Brazil, and Spain.
Mpox (Monkeypox) transmission
Mpox is spread either through close contact with infected people or animals or by contact with contaminated materials, such as sheets, medical materials, or clothes.
The most infectious are skin lesions transmitting the virus skin to skin, often during sexual activities. Air transmission is also possible in very close contact.
A person is contagious from the onset of symptoms until the rash is fully healed and the skin renewed. Limited data suggest the possibility of transmission one to four days before the symptoms arise.
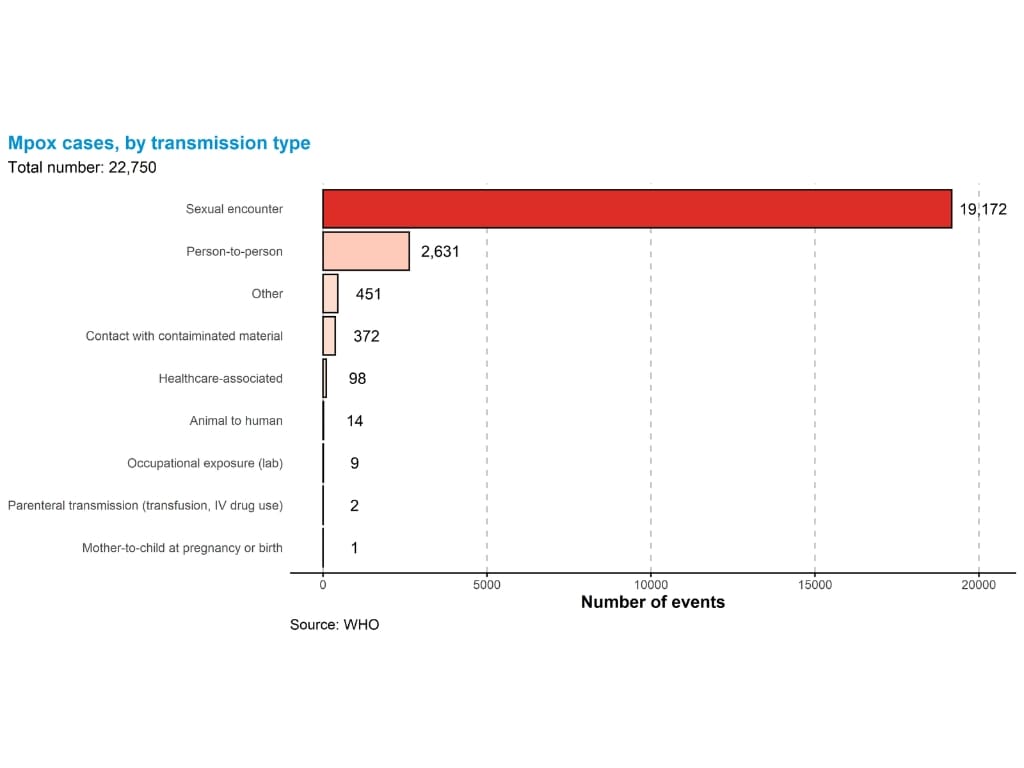
Although there are many ways of getting infected, sexual transmission is the most frequent one.
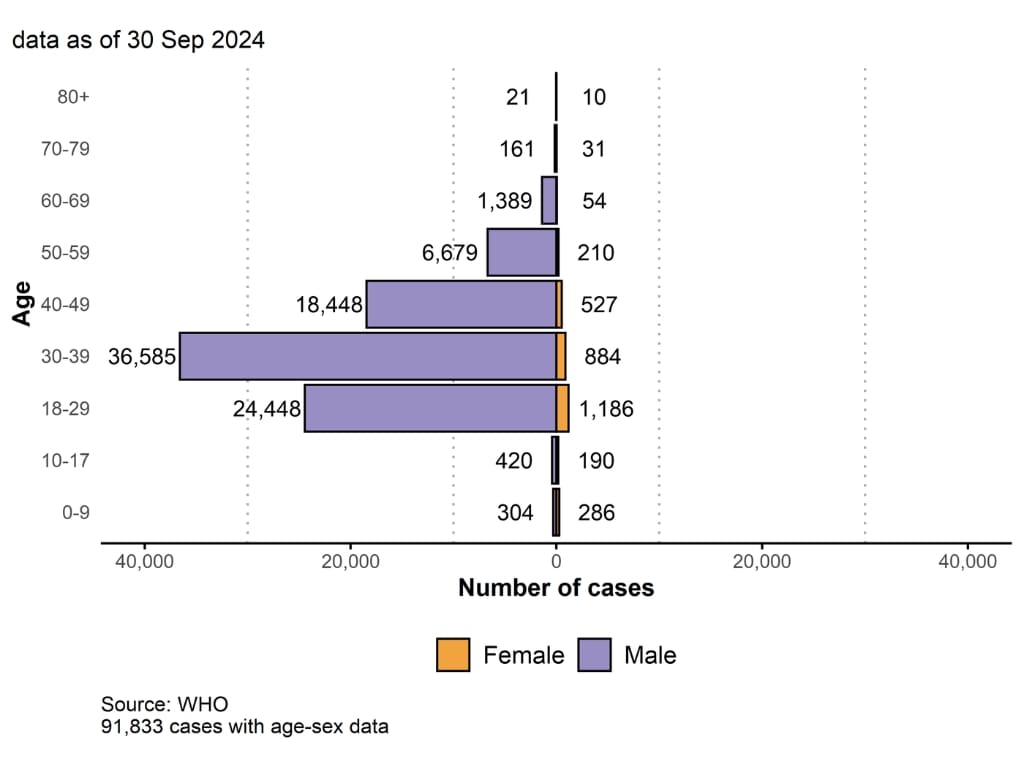
In both Clades, 96% of cases were male, and in cases where data were available, 84.9% were men who have sex with men.
Mpox (Monkeypox) symptoms
There are various presentations of the disease.
After an incubation period (the time between acquiring the virus and the onset of symptoms) of 3 – 17 days, flu-like syndrome can occur, with symptoms like fever, headache, sore throat, or malaise accompanied by lymph node swelling in one or more locations.
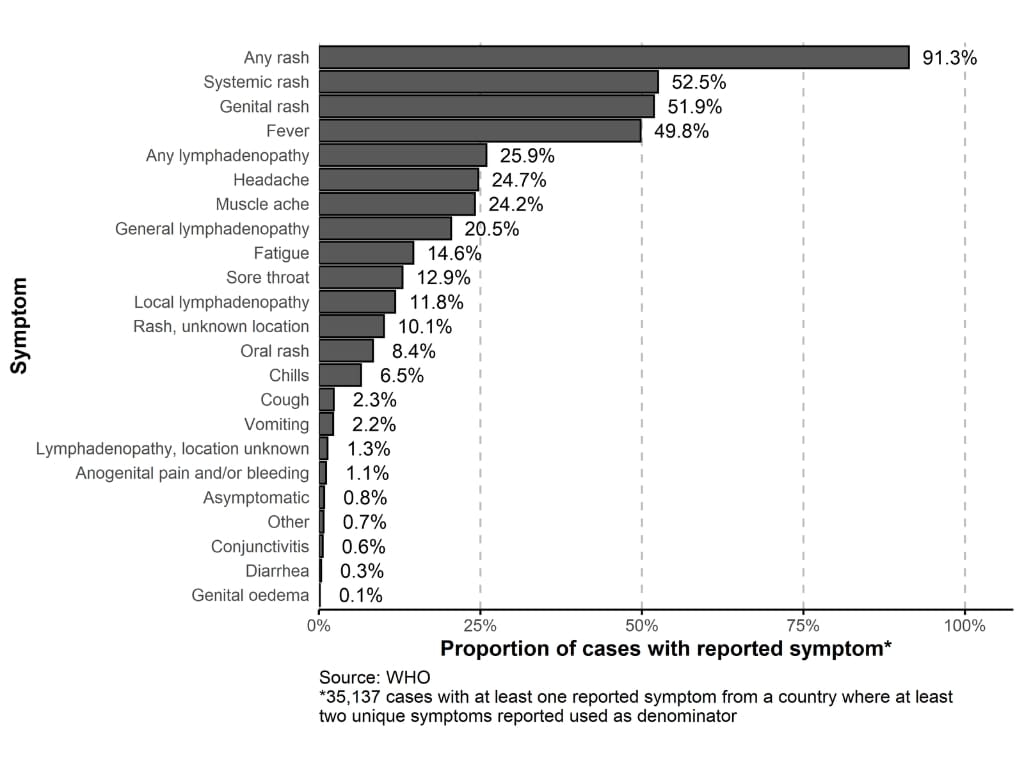
Then, a rash will start to form and change its appearance in time. Initially, it can look like pimples or blisters, then it scars and goes from painful to itchy.
There can be few or hundreds of these skin lesions anywhere on the body but often in the place of transmission (palms, face, mouth, genitals, anus, etc.)
Mpox symptoms will typically last 2-4 weeks.

Mpox (Monkeypox) treatment and vaccination
No special treatment for Mpox is available.
Experimental antiviral therapy is occasionally used in people with a high risk of severe disease. (pregnant, children, immunocompromised) Vaccine applied less than 4 days (sometimes more) after a risk contact may reduce severity of symptoms.
A safe vaccine is available and is expected to be effective against both Clades of Mpox.
Current recommendations for both non-travelers and travelers are based on sexual risk assessment.
Two doses of the JYNNEOS vaccine 4 weeks apart are recommended to these travelers to countries with recent Clade I Mpox cases (Burundi, Central African Republic, Democratic Republic of the Congo, Republic of the Congo, Rwanda, and Uganda):
Anticipating sex with a new partner, sex at a sex club or similar venue, sex in exchange for money or other things, sex associated with public events, parties, festivals, raves, etc. This includes all forms of sex, and it’s not gender specific.
This is the CDC recommendation. The UK doesn’t recommend the vaccine to travelers other than humanitarian and health workers.
Current Mpox (Monkeypox) outbreak in DRC
Although Mpox occurs regularly in DRC, the current outbreak is more widespread than any previous DRC outbreak and has spread to neighboring countries.
In August 2024, it was declared a Public Health Emergency of International Concern (PHEIC) by WHO. In October, the Global Health Emergency corps were activated to support affected countries, mainly DRC.
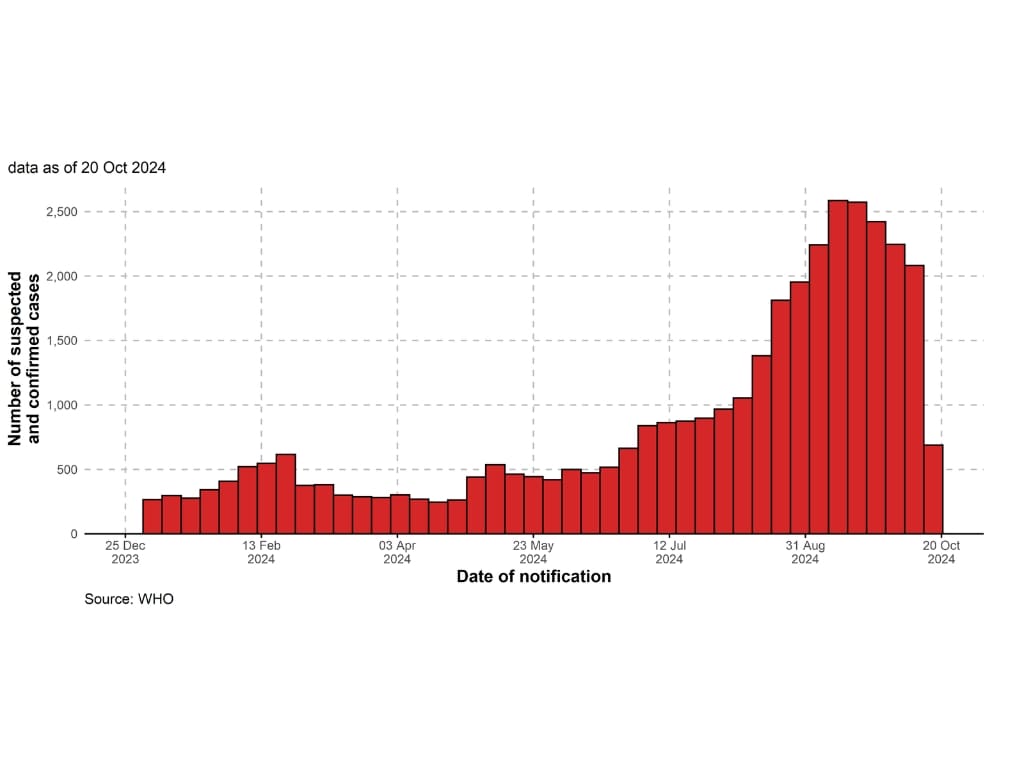
Due to limited testing availability and security problems, it’s hard to get exact numbers of cases. However, it looks like the outbreak in DRC and neighboring countries is not getting under control anytime soon.
Mpox (Monkeypox) risk for travelers
The risk to the general population, including travelers, remains low.
Travelers should follow this advice to stay safe and further reduce the risk of transmission:
Avoid close contact with people who are sick, presenting any of the symptoms, and especially with visible skin lesions. (hugs, kisses, cuddle, sex)
Avoid contact with wild animals in Mpox-endemic areas, including eating or using any products from them.
Avoid contact with any materials that might be contaminated by people or wild animals that are sick.
Wash your hands with soap often and always before eating and touching your face.
Consider minimizing skin-to-skin contact with others (parties, raves)
If you travel to any of the countries (Burundi, Central African Republic, Democratic Republic of the Congo, Republic of the Congo, Rwanda, and Uganda) and develop a rash, with or without other symptoms, seek medical care, but isolate yourself first until the Mpox disease is confirmed or ruled out. If you think you might have Mpox, see detailed advice here.
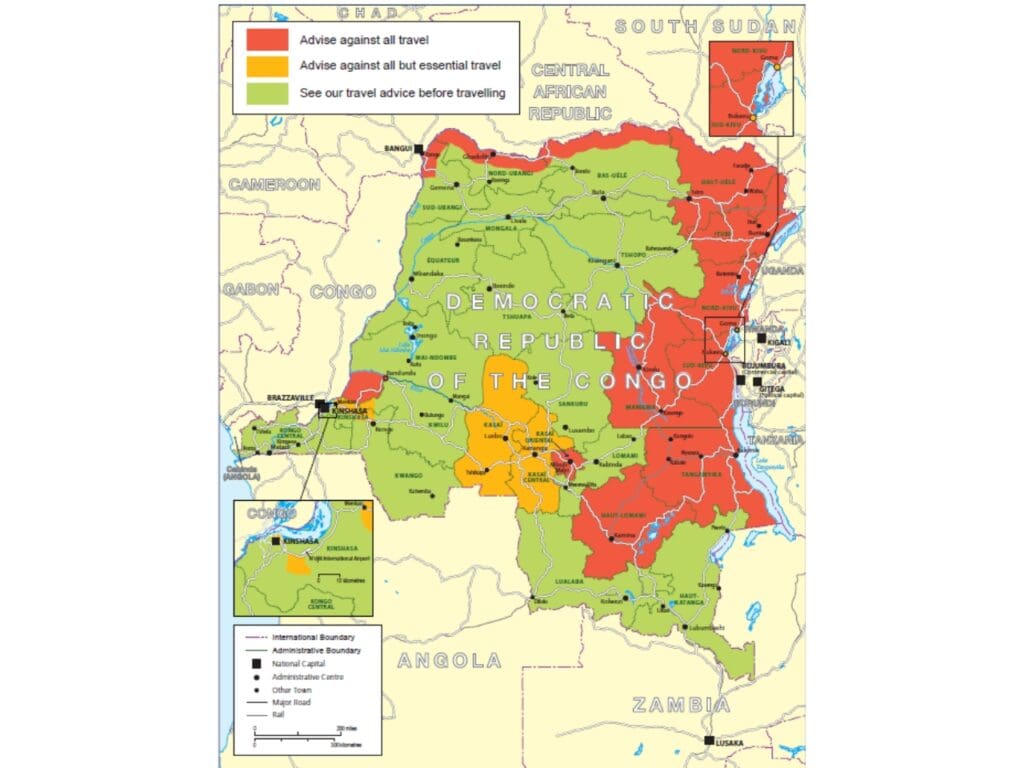
Although health risk from the Mpox outbreak remains low for the average traveler, US, UK, and Australian institutions put most parts of DRC in a level 3 or level 4 bracket, which advises against all but essential travel or against all travel, respectively. This is due to crime, civil unrest, and armed conflict in some regions.
Other countries where Mpox is spreading and are safer for tourists, like Rwanda or Uganda, have level 2 Notices by the CDC, which means enhanced precaution.
Considering the way of transmission, number of cases, and average travelers following the advice, Mpox shouldn’t be a reason for not traveling here.
Resources
2022-24 Mpox Outbreak: Global Trends. Geneva: World Health Organization, 2024. Available online: https://worldhealthorg.shinyapps.io/mpx_global/
https://www.cdc.gov/mpox/about/
https://www.cdc.gov/mpox/caring/index.html
https://www.cdc.gov/mpox/hcp/clinical-signs/index.html
https://www.cdc.gov/mpox/outbreaks/2022/index-1.html
https://www.cdc.gov/mpox/outbreaks/2023/index.html
https://emergency.cdc.gov/han/2024/han00516.asp
https://wwwnc.cdc.gov/travel/notices/level2/clade-1-mpox-central-eastern-africa
https://www.cdc.gov/poxvirus/mpox/vaccines/vaccine-recommendations.html
https://www.ecdc.europa.eu/en/mpox
https://travelhealthpro.org.uk/news/792/mpox-outbreak-in-africa-clade-i-mpox-virus-infection
https://www.canada.ca/en/public-health/services/diseases/mpox/outbreak-update.html
https://www.cdc.gov/mpox/travel/index.html
https://www.gov.uk/foreign-travel-advice/democratic-republic-of-the-congo
https://www.smartraveller.gov.au/destinations/africa/democratic-republic-congo
Disclaimer:
The information provided in this blog post is for general informational and educational purposes only and is not a substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any health problem. The use or reliance on any information provided in this blog post is solely at your own risk.