Dengue fever is a viral disease spread by mosquitos. Travelers to popular tropical and subtropical destinations have been at increased risk of infection in recent decades, especially with the recent rise in cases across Latin America, Asia, and beyond.
This guide provides essential information about dengue fever symptoms, risk levels, recent outbreaks, and proven strategies to avoid infection.
Equip yourself with the knowledge you need to travel safely and responsibly—don’t let dengue fever ruin your next adventure!
In This Article
This post includes affiliate links. If you choose to purchase through these links, I may receive a commission, helping me continue creating valuable content for you. This comes at no additional cost to you.
What is Dengue Fever?
Dengue fever is a viral infection transmitted by the Aedes mosquito endemic in over 100 countries. It typically thrives in tropical and subtropical climates worldwide, mostly in urban and semi-urban areas.
Historically, after spreading from Africa, approximately 70% of cases were reported in Asia. That changes now with large outbreaks in Central and Latin America.
There are four related serotypes (DENV-1 to DENV-4). After getting infected, immunity is lifelong but limited only to the same serotype. Protection against others wanes over time, and after 2-3 years, infection with a different serotype results in a much higher chance of severe Dengue than the first infection.
Around two-thirds of Dengue infections are asymptomatic. When symptomatic, it typically presents as an acute febrile illness. 1 – 3% of dengue cases are severe and potentially life-threatening.
Dengue results in death in under 0.1% of all cases. In endemic countries, children and infants are primarily affected by severe and deadly cases, and therefore, numbers might be different in travelers.
Where is Dengue Most Prevalent?
Dengue fever is the most widespread mosquito-borne illness. According to WHO estimates, the risk of Dengue is present in over 132 countries with 3.9 billion people (half of the world population) and modeled estimates of 390 million infections, 96 million symptomatic cases, and 40,000 deaths annually worldwide.
Recently, it overtook Malaria, for which 3.3 billion people are at risk; it causes an estimated 249 million cases and more than 608,000 deaths annually worldwide.
I must note that the estimates and confirmed cases differ greatly for many reasons (e.g., the large percentage of asymptomatic cases, the lack of reporting by healthcare facilities, etc.).
In contrast to Malaria, Dengue is on the rise. In fact, the number of annual cases is rising faster than any other infectious disease!
From 2000 to 2019, the WHO documented a tenfold surge in reported cases, increasing from 500,000 to 5.2 million.
After a 2019 peak and then a slight decline between 2020 and 2022 due to the COVID-19 pandemic, dengue cases surged in 2023 to 6.5 million, and in 2024, there were already over 14 million Dengue cases and over 10,000 Dengue-related deaths reported.
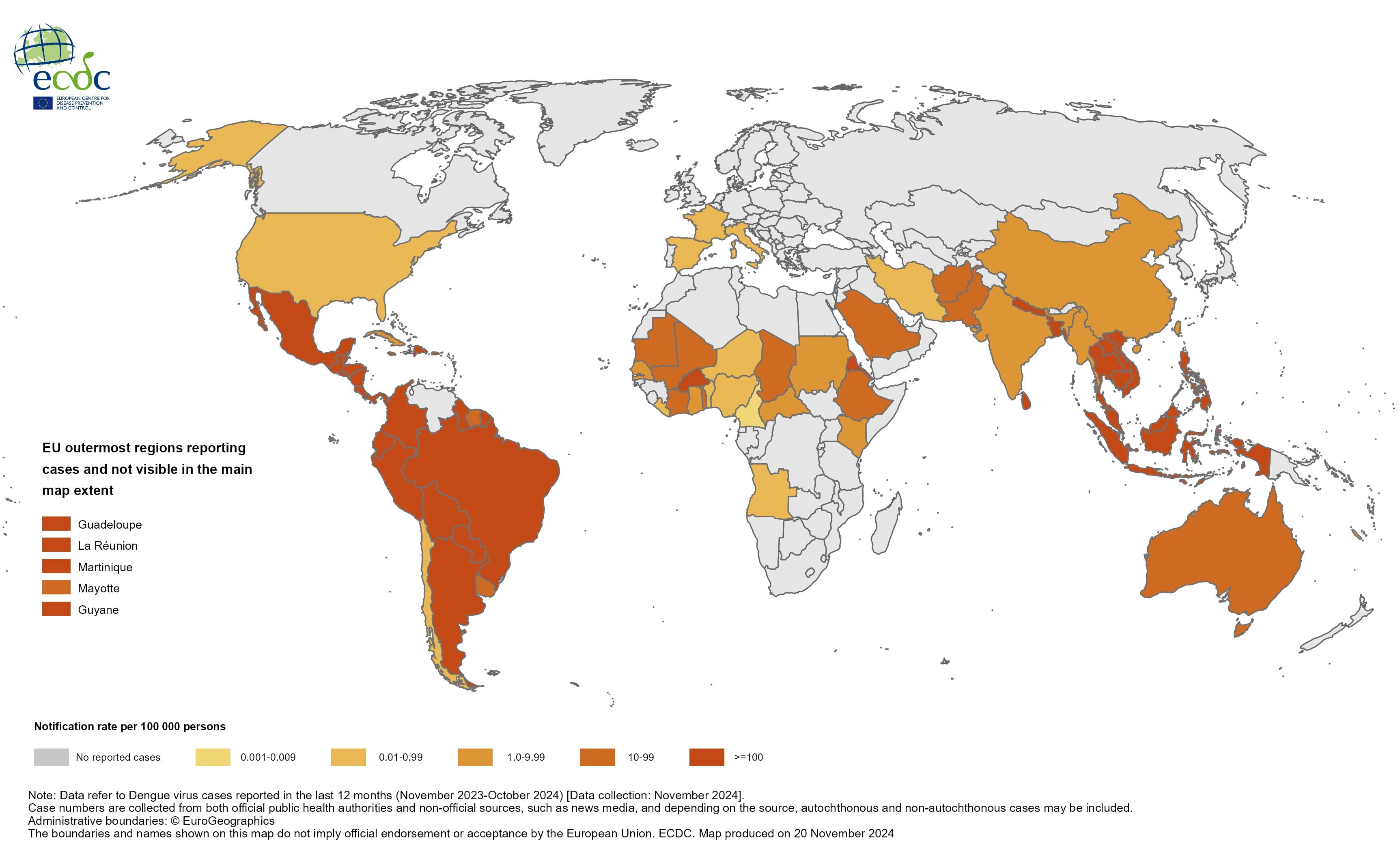
In 2023, almost 80% of the cases have been reported in South and Central America, with Brazil by far the first in number of cases worldwide (3,088,723), followed by Vietnam (369,000), Bangladesh, Mexico, and Peru. But it was not just Latin America that was fighting an outbreak. Thailand also saw a steep rise in cases (over 300% compared to 2022).
There are several reasons for the extreme rise in Dengue. Mainly, it is climate change, urbanization, the El Niño phenomenon (heavy rainfall, high humidity, and higher temperatures in Latin America), and political and humanitarian crises in some countries.
You can find the latest information about potential outbreaks in the area you travel on this website.
Transmission: How Do Travelers Get Dengue?
The virus is transmitted through the bite of an infected mosquito called Aedes. Mainly, it’s Aedes aegypti and Aedes albopictus. This mosquito is very different from Anopheles, which transmits malaria or other mosquitoes in Europe or North America.
Aedes aegypti prefers human blood to animal blood. It’s most active during the day and is adapted to urban and semi-urban areas. In addition to Dengue, it spreads Zika, Chikungunya, and Yellow fever.
The presence of the mosquito doesn’t necessarily mean it contracts any of the diseases. For example, Yellow fever is not present in Asia, but these countries have strict requirements when entering from some African countries where this virus circulates. That’s because the virus could be introduced to the country where the mosquito already lives.

Peaks of dengue infections are seasonal based on the local climate, but lately, region-specific outbreaks have played an important part in the risk of transmission.
Traditionally, peak months were March for South America, August and October for the Caribbean, June and September for Southeast Asia, and October for South Asia. Nowadays, the situation is changing quickly, with large outbreaks in Brazil and other countries in South America and uncertainty around the underreporting of cases in Sub-Saharan Africa.
Local transmission of Dengue was reported in many countries of Europe, as well as in the US, namely in Madeira (Portugal), Texas, and Florida. Altough the risk remains very low for now, because of climate change the spread of Dengue in the Northern hemisphere might be a concern in near future as Aedes aegypti is already established in 167 countries and cases and the volume of travel are rising each year.
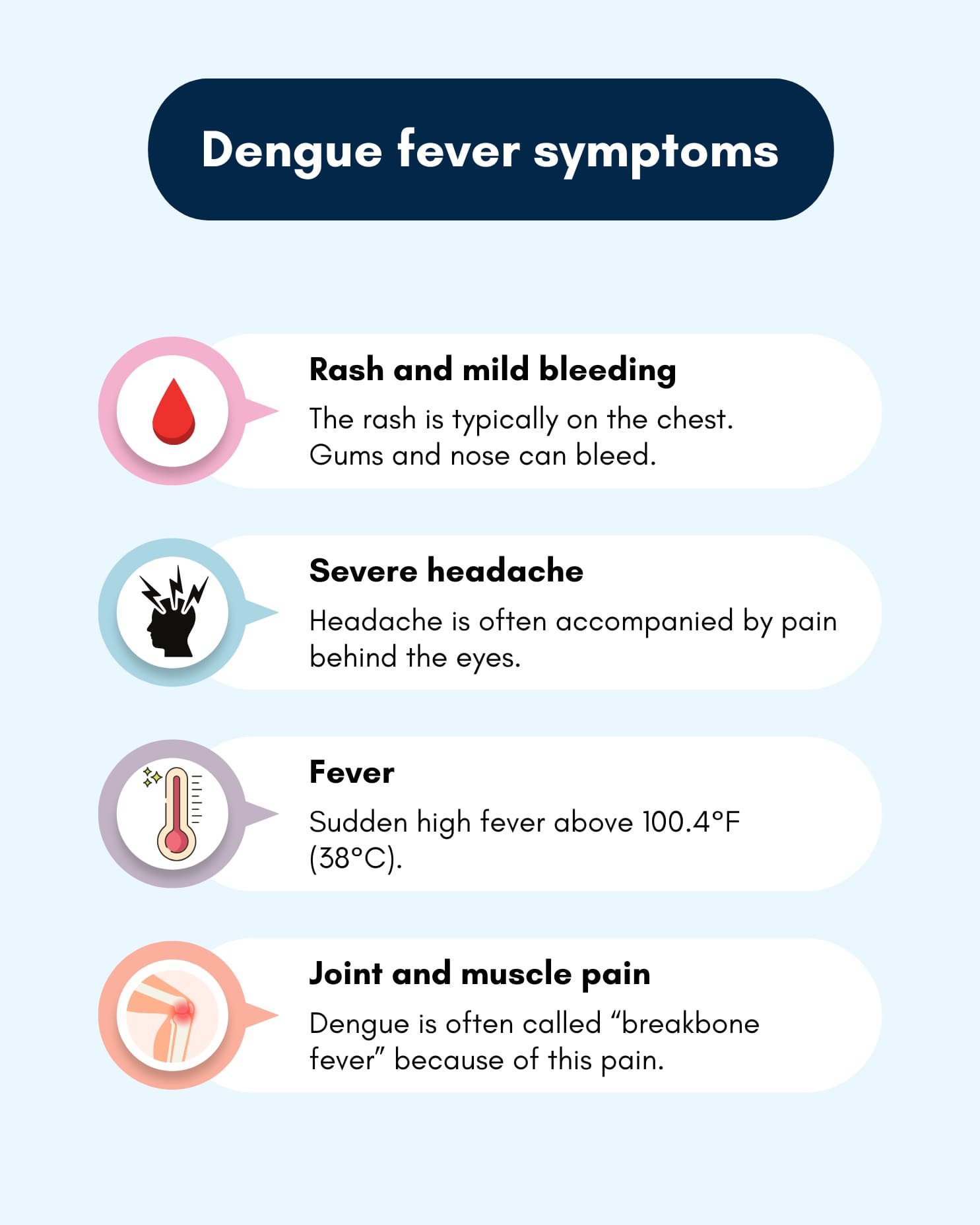
Symptoms: How to Recognize Dengue Fever
40 – 80% of dengue infections go unnoticed. In travelers, it’s probably on the higher end (75% in a study on US travelers). This might be either because the second infection tends to be more often symptomatic and severe, and many travelers might not have a chance to get infected twice, or because most travelers are adults, while in the local population, infants, children, or people over 65 are the worst affected.
If you’re in that unlucky 25%, symptoms will show in 4-7 days after getting infected, although it can be as long as 14 days. Many travelers will become sick after returning home (36% of travelers).
Typically, you’ll experience mild to moderate symptoms like:
- Sudden high fever
- Severe headache
- Pain behind the eyes
- Joint and muscle pain (often called “breakbone fever”)
- Rash and mild bleeding symptoms (easy bruising, nose or gum bleeding)
In 1%-3% of the cases, severe illness will manifest in three phases.
- Febrile phase:
High fever and other symptoms described will last for 2-7 days. - Critical phase:
This happens when you’re not getting better after having a fever, and the illness progresses with abdominal pain, difficulty breathing, restlessness or severe fatigue, and vomiting. This phase typically begins when the temperature decreases, and many patients will improve in 24-48 hours.
Some patients, however, will further progress by losing volume in the circulation, causing hypotension, shock, and, in some cases, death. Some patients might lose blood in stool, vomit, and even by bleeding from the uterus. Convalescent phase:
If the leak of the plasma from circulation stops or the patient is supported by IV solutions, the blood pressure settles, and the patient improves. The rash can worsen and get itchy but other than that the full recovery is expected in 1-2 weeks.
In 2023, the case-fatality ratio (percentage of deaths from confirmed cases) was 0.05% in South America and 0.22% in Asia.
In mild and moderate cases, the fever lasts a few days, but in some adults, tiredness, weakness, and muscle pain can persist for weeks or even months.
What to Do if You Suspect Dengue
There is no specific treatment for Dengue. Mild cases are usually handled by drugs that tackle fever and pain. In severe cases, intravenous fluids are the main weapon, effective in most cases.
If you begin to experience dengue symptoms while traveling:
- Rest and hydrate as much as possible
- Use painkillers and drugs that decrease fever, ideally acetaminophen (paracetamol). Use physical cooling with a wet sponge or cloth. Don’t use non-steroidal anti-inflammatory drugs, like ibuprofen and aspirin, or any drugs that contain these, as they increase the risk of bleeding. Seek medical attention if you use any anticoagulant for any condition.
- Seek medical help if you experience severe symptoms, including persistent vomiting, abdominal pain, difficulty breathing, or signs of shock. Intensive supportive care, including IV fluids, can reduce mortality (death rate) by 20-fold when managed correctly. The critical phase usually starts on day 4 or 5 of the illness. Seek medical attention after having a fever over 3 days.
- Avoid mosquito bites by net or repellent to reduce the risk of further transmission
If you think you might have Dengue fever after returning home, make sure to mention when and where you’ve traveled.

How Dangerous is Dengue for Travelers?
Travelers to dengue-endemic regions face a measurable risk, with an estimated 2.8 cases per 100,000 travelers (based on a study on European travelers between 2015 and 2019). However, this risk is highly variable and depends on the destination, season, activities, duration of stay, and current outbreaks.
For instance, travelers to Southeast Asia and Latin America experience significantly higher infection rates than those visiting Africa. An example from European imported cases in 2022 shows the importance of outbreaks. The most travel-related cases were in travelers to Cuba (37%), where a large outbreak occurred.
As Dengue occurs mostly in urban areas, business travelers are also at risk, even on short-term travel. The risk, however, rises with the duration of the stay. In a study on US travelers, 7% had positive antibodies (meaning they contracted the virus) when traveling longer than 2 weeks but less than a year, and 40% in those traveling more than a year.
In another study, US travelers to endemic countries for the median length of 3 weeks returned with positive antibodies between 2.9% and 6.8%. Just a quarter of these travelers had symptoms.
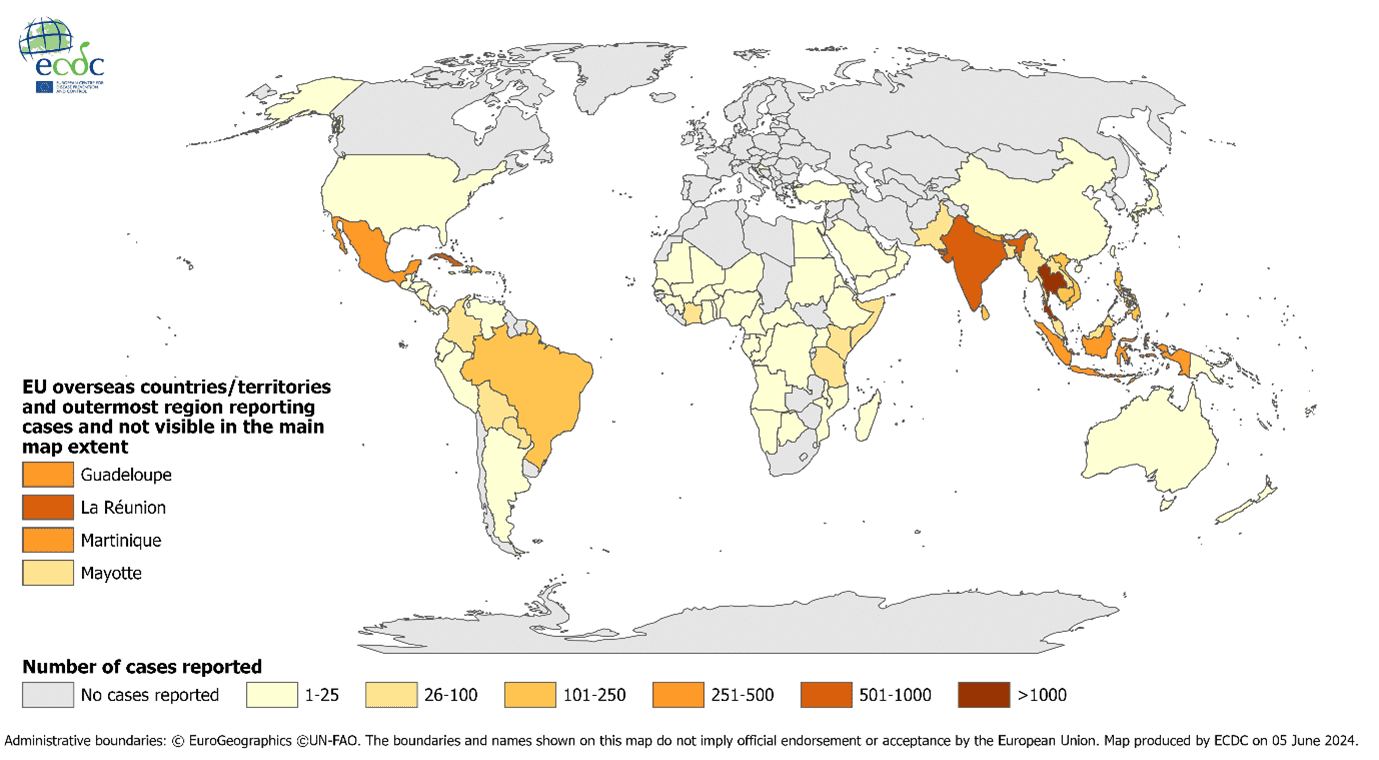
Dengue has become the leading cause of fever in returning travelers from Southeast Asia, surpassing Malaria. The number of hospitalizations and the proportion of Dengue cases in ill-returned travelers has been rising fast in the last two decades.
There were 82,825 ill Western travelers reported to GeoSentinel (a network of travel medicine centers) in the years 1996-2011; there were 1,910 patients with Dengue, 18 with severe Dengue, and one death was recorded due to severe dengue.
Dengue is a frequent cause of travel illness, more frequent than hepatitis A and B, Japanese encephalitis, and others. It might affect your travel plans and can result in high costs in case of insufficient travel insurance. Severe dengue and deaths remain rare.
Prevention: Essential Tips to Avoid Dengue Fever
There’s no guaranteed way to prevent Dengue fever, but travelers can greatly reduce their risk with these precautions:
- Use Repellent:
Apply insect repellent containing DEET (ideally 30% or more) or picaridin, especially during peak mosquito hours, that is early morning and late afternoon for the Aedes species - Wear Protective Clothing:
Long sleeves and pants in light colors provide a barrier against bites. Permethrin or other treatments for clothing add to effectivity - Choose Safe Accommodations:
Stay in rooms with screened windows, air conditioning, or mosquito nets. Use mosquito-repellent devices or spray the surfaces inside your room with repellent. - Eliminate Standing Water:
If you stay longer or plan to live in a new place, avoid stagnant water where mosquitoes can breed. (flowerpots, water tanks…)
These strategies are critical in high-risk areas, especially in Latin America and Southeast Asia, where dengue transmission rates are high.

Should You Consider Dengue Vaccination?
Currently, two vaccines are available: Dengvaxia® and Qdenga®.
Dengvaxia® is used only for those with a confirmed history of dengue infection, as it can increase the risk of severe dengue in those without prior exposure. It’s also used in areas with a high risk of Dengue but only for the local population.
Qdenga®, approved by the European Medicines Agency (EMA), offers broader protection, but it’s most effective for individuals who have had dengue before. It’s not available in the US.
For travelers, vaccination may be advised based on individual risk, travel length, and destination. The Qdenga® vaccine may be considered for those visiting high-risk areas for extended periods (over six weeks). However, due to limited efficacy in older adults and those without prior infection, travelers should discuss vaccination with a healthcare professional.

Guidelines in the UK recommend this vaccine only for travelers previously infected. That might be often hard to assess as up to 80% of infections present no symptoms and blood test can be false positive after contracting similar viruses, such as Zika or even vaccination against yellow fever, Japanese encephalitis or tick-borne encephalitis.
Dengue vaccination, along with other vaccines, is explained in a separate article.
Summary
Dengue fever is a growing concern for local populations as well as for travelers, especially in Latin America and Southeast Asia. With over 14 million confirmed cases worldwide in 2024, it’s essential to stay informed, take preventive steps, and know when to seek medical care.
Use repellents, wear protective clothing, and consider vaccination if you’re at high risk. Don’t let dengue fever spoil your travel plans – stay safe, stay informed, and make the most of your adventures.
Resources
Lancet, T. (2024). Dengue: the threat to health now and in the future. Lancet (London, England), 404(10450), 311.
Travel Medicine, 4th Edition – December 13, 2018, Authors: Jay S. Keystone, Phyllis E. Kozarsky, Bradley A. Connor, Hans D. Nothdurft, Marc Mendelson, Karin Leder, Language: English, Hardback ISBN: 9780323546966
Centers for Disease Control and Prevention (CDC). (2023). CDC Yellow Book 2024: Health Information for International Travel. Oxford University Press.
Wilder-Smith, A., Ooi, E. E., Horstick, O., & Wills, B. (2019). Dengue. The Lancet, 393(10169), 350-363.
Haider, N., Hasan, M. N., Onyango, J., & Asaduzzaman, M. (2024). Global landmark: 2023 marks the worst year for dengue cases with millions infected and thousands of deaths reported. IJID Regions, 13, 100459.
Halstead, S., & Wilder-Smith, A. (2019). Severe dengue in travellers: pathogenesis, risk and clinical management. Journal of travel medicine, 26(7), taz062.
Sanchez-Vegas C, Hamer DH, Chen LH, et al. Prevalence of dengue virus infection in US travelers who have lived in or traveled to dengueendemic countries. J Travel Med 2013; 20(6): 352-60.
Olivero RM, Hamer DH, MacLeod WB, et al. Dengue Virus Seroconversion in Travelers to Dengue-Endemic Areas. Am J Trop Med Hyg 2016.
Jensenius M, Han PV, Schlagenhauf P, et al. Acute and potentially life-threatening tropical diseases in western travelers–a GeoSentinel multicenter study, 1996-2011. The American Journal of Tropical Medicine and Hygiene 2013; 88(2): 397-404.
Franklinos, L. H., Jones, K. E., Redding, D. W., & Abubakar, I. (2019). The effect of global change on mosquito-borne disease. The Lancet infectious diseases, 19(9), e302-e312.
Laporta, G. Z., Potter, A. M., Oliveira, J. F., Bourke, B. P., Pecor, D. B., & Linton, Y. M. (2023). Global distribution of Aedes aegypti and Aedes albopictus in a climate change scenario of regional rivalry. Insects, 14(1), 49.
Martin Angelin, Jan Sjölin, Fredrik Kahn, Anna Ljunghill Hedberg, Anja Rosdahl, Paul Skorup, Simon Werner, Susanne Woxenius, Helena H. Askling, Qdenga® – A promising dengue fever vaccine; can it be recommended to non-immune travelers?, Travel Medicine and Infectious Disease, Volume 54, 2023, 102598, ISSN 1477-8939, https://doi.org/10.1016/j.tmaid.2023.102598
Menon, S., Wilder-Smith, A. New Vaccines on the Immediate Horizon for Travelers: Chikungunya and Dengue Vaccines. Curr Infect Dis Rep 25, 211–224 (2023). https://doi.org/10.1007/s11908-023-00811-x.
Eperon, G., Veit, O., Antonini, P., Fehr, J., Haller, S., Hatz, C., Landry, P., Neumayr, A., Niederer-Lohrer, A., Schlagenhauf, P., de Vallière, S., Staehelin, C., & on behalf of the Swiss Expert Committee on Travel Medicine (ECTM). (2024). Vaccination against dengue fever for travellers: Statement of the Swiss Expert Committee for Travel Medicine, an organ of the Swiss Society for Tropical and Travel Medicine, August 2024. Swiss Medical Weekly, 154(9), 3858 . https://doi.org/10.57187/s.3858
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/dengue
https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
https://www.ecdc.europa.eu/en/dengue-monthly
https://www.ecdc.europa.eu/en/dengue/surveillance/dengue-virus-infections-travellers
https://www.ecdc.europa.eu/en/publications-data/dengue-annual-epidemiological-report-2022
https://www.ecdc.europa.eu/en/disease-vectors/facts/mosquito-factsheets/aedes-aegypti
Disclaimer:
The information provided in this blog post is for general informational and educational purposes only and is not a substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any health problem. The use or reliance on any information provided in this blog post is solely at your own risk.