The typical question of a traveler regarding vaccination is:
What vaccine do I need in Thailand? Or should I get this vaccine for Bali? Or, I’m leaving for Mexico in a week; should I get any vaccine?
If only it were this easy. The destination alone can only help us determine what vaccine we do not need when the infection is not present there. It doesn’t work the other way around.
The fact that the infectious disease occurs in the country doesn’t imply that everyone traveling there should get vaccinated against it. This might be the most important idea in this post.
In This Article
Disclaimer:
The information provided in this blog post is for general informational and educational purposes only and is not a substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any health problem. The use or reliance on any information provided in this blog post is solely at your own risk.
From the perspective of the pathogen, there are factors like:
- mode of transmission
- whether it needs a vector (mosquito, tick, etc.)
- how infectious it is
- what illness it causes
- whether it is seasonal or all year round
- whether it is limited to the forest area or thrives in places with dense human populations
From the traveler’s perspective, we need to consider:
- conditions such as diabetes, obesity, asthma, etc.
- age
- immunocompromising illness or drugs
- pregnancy
- the planned itinerary, including the time of year and activities
- potential adverse effects and costs of the vaccine are also taken into account
The bottom line is that a travel health clinic professional will recommend the vaccines based on your needs.
I could end this post here, but instead, I tried to divide the most used vaccines based on the factors I just named. Remember, this is just to orient better, not make informed decisions. Let’s dive in.
All travelers – routine vaccines
All developed countries have a set of routine vaccinations and a calendar of recommended times for application from birth to adulthood. Some are more relevant at a young age, and some try to induce collective immunity or even eradication.
Embarking on a journey to places with different weather and hygienic conditions might be a perfect opportunity to catch up on vaccinations against infections present worldwide, but much more in developing countries with weak vaccination programs.
Recommended routine vaccinations are:
MMR vaccine (Measles, mumps and rubella)
Sadly, there is falling MMR coverage due to antivaccine movements and COVID-19 disruption, and sporadic outbreaks occur in the US and Europe.
These diseases are much more common in developing countries, putting travelers in a position to import the disease back home.
From the trio, Measles has the potential for the most severe complications, such as pneumonia, encephalitis, etc.
All travelers should have received at least two doses of modern MMR vaccines.
The use of these vaccines differs by country, but in general, people born before 1980 should consult a professional about the type of vaccine they got and potentially get vaccinated with a modern vaccine if needed.
Diphtheria, Tetanus, Pertussis (Whooping cough) vaccine
All travelers should be up to date with these vaccines, including boosters based on age and last dose.
Tetanus is particularly important, as all travelers have a higher risk of injuries, animal bites, etc.
In many countries, Tetanus is the only booster adults are getting, leaving them unprotected against Diphtheria and Pertussis.
Travelers should get the Tdap vaccine every 10 years. (Includes all three in one shot).
Tdap + polio in a single vaccine might be useful for some travelers, but it’s currently not available for adults in the US. It is available in Canada, Australia and most European countries.
Varicella (Chickenpox) vaccine
Nonimmune adult travelers should strongly consider Varicella vaccination because it can be severe in adults (pneumonia, etc.).
US criteria for varicella immunity are: (at least one needs to be met)
- being born in the United States before 1980
- two doses of varicella vaccine
- physician-diagnosed acute chickenpox or shingles
- laboratory evidence of immunity
Influenza vaccine
CDC recommends the yearly flu vaccine for everyone older than 6 months.
The highest risk of severe illness and death is in children younger than 2 years of age and adults over 65 years old. Other risk groups are pregnant women, oncologic patients, diabetics, patients with chronic lung disease, and others.
Influenza season starts around October in the northern hemisphere and lasts from April to September in the southern hemisphere. In the tropics, influenza is present all year.
Most travelers
Hepatitis type A vaccine
Hepatitis type A is one of the most common infections in travelers preventable by vaccine.
Transmission is most often caused by contaminated food and water. 70% of adults develop jaundice, and approximately 10% of these patients can have symptoms for over 6 months.
All travelers older than 1 year traveling to countries with intermediate and high prevalence (presence) should be vaccinated.
The first dose can be applied as late as on the day of departure to protect you. After the booster dose in 6 – 36 months, lifelong protection is expected.
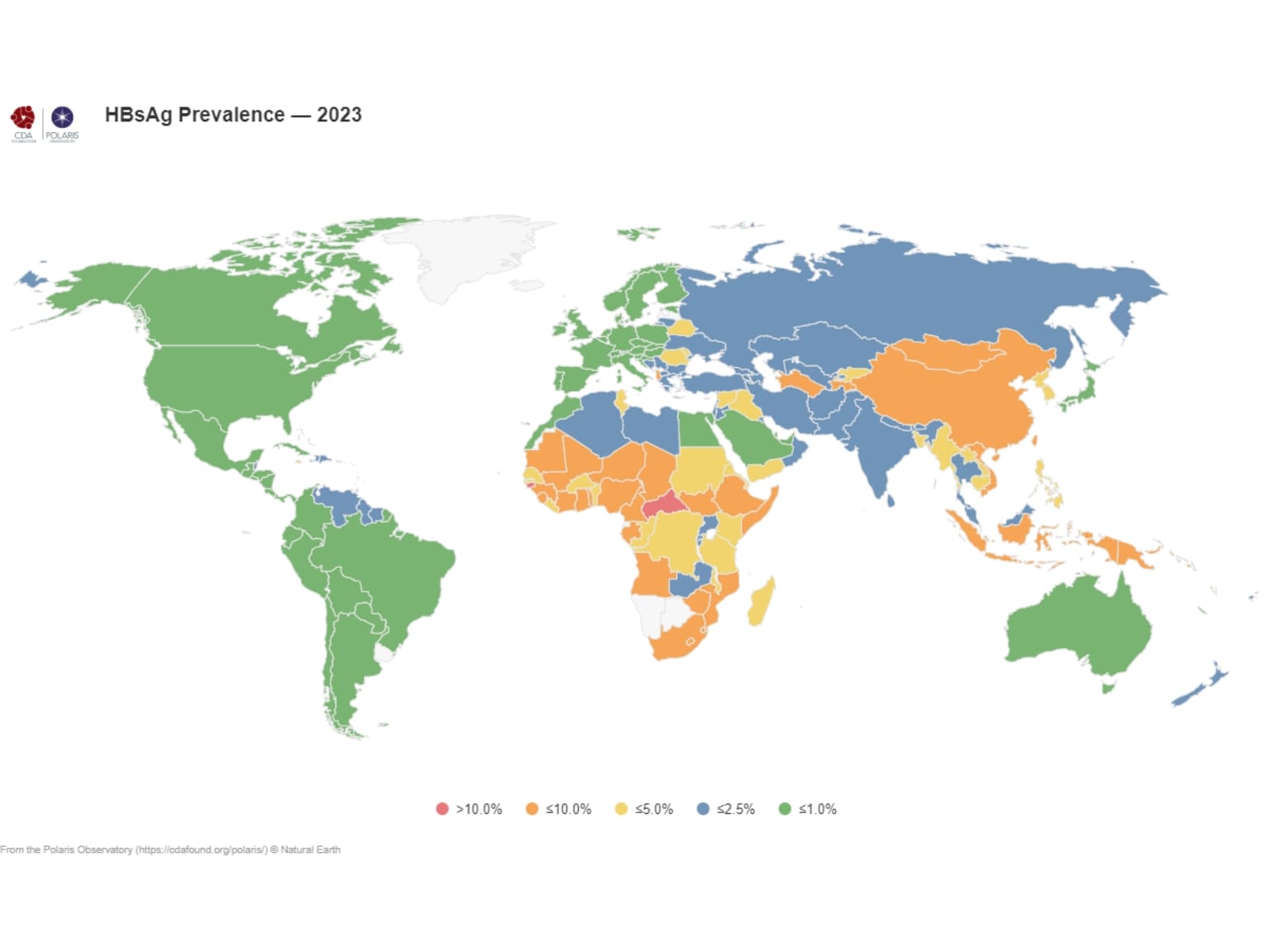
Hepatitis type B vaccine
It’s estimated that 2 billion people have been infected, and 240 million have chronic infections affecting the liver. 686,000 people die every year due to the consequences of the disease.
It’s transmitted by blood and other body fluids of an infected person. The virus is 50 – 100 times more infectious than the HIV virus!
Due to the high risk of injuries potentially resulting in medical or dental care abroad (60% of travelers’ health issues are injuries and traffic accidents) and the character of the disease, WHO recommends hepatitis B vaccination to all travelers to intermediate and high-risk areas.
Three doses are needed in 6 months’ time to achieve life-long protection. A person is protected after the second dose, which is applied a month after the first.
The Twinrix® vaccine combines Hepatitis A and B. Instead of five shots, only three are needed.
Vaccines against Hepatitis A and B are well tolerated, offer lifelong protection, and are, therefore, medically and economically a great choice and a bare minimum for all travelers.
Typhoid vaccine
Typhoid fever is caused by the bacteria Salmonella typhi. It occurs worldwide, but it’s mostly associated with poor sanitation in warm climates. People can get the infection from contaminated food and water, and once they are infected, they spread the bacteria in the environment.
The highest risk of getting sick is in the Indian subcontinent, then South East Asia. Some African countries pose a moderate risk. The risk is also higher in travelers who eat and travel more adventurously, in remote areas, or in close contact with the local population.
The vaccination is available in injection (single dose) – Typhim®, Typherix®, and capsule form – Vivotif® (4 capsules in 7 days). The expected protection is three years for the injectable form and 5 to 7 years for the oral vaccine.
Other preventive measures still need to be followed, as the efficacy of both vaccines is around 50%. It should be administered no later than 14 days before departure.

Frequent or long-term travelers
Rabies vaccine
Rabies is a viral infection affecting the nervous system and attacking the brain. Once the symptoms arise, it ends in death in almost 100% of cases.
Practically all the transmission to humans occurs after dog bites, and almost all deadly cases happen in Africa and Asia. The death toll is estimated at around 59,000 people every year, although the real number might be much higher.
Rabies in travelers is rare. However, bites and scratches from potentially rabid dogs in areas where rabies is common are quite frequent.
Because of the deadly nature of the virus and the difficulty of determining the status of the animal, travelers are often treated as if the rabies were present to prevent the worst-case scenario. The probability of this is approximately 0.4 % per month of stay. That includes bites and scratches from monkeys.
After the injury, local doctors will usually recommend post exposition prophylaxis, which means preventing the development of the disease even after the transmission.
It consists of 4 doses of the vaccine on days 0, 3, 7, and 14. In some cases, 5 doses are needed. Special immunoglobulin (injection of already-made antibodies) is also required. However, if the person has already been vaccinated, just two vaccine applications are needed, with no immunoglobulin.
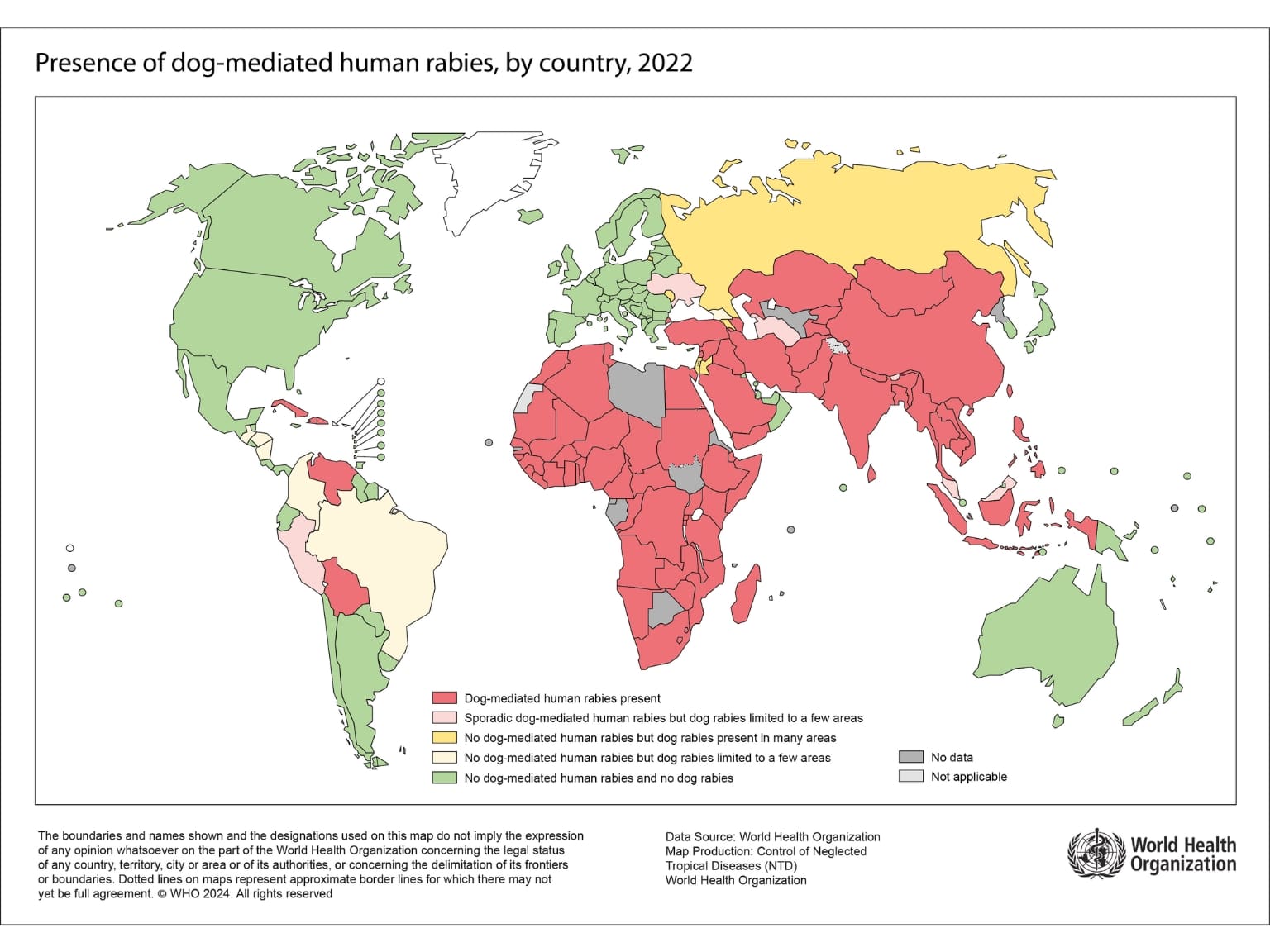
Not just the cost and length of the treatment are in the equation. There is also a problem with the availability of the treatment.
Besides modern CCV (cell-culture vaccines) like Verorab® and Rabipur®, older DEV (duck embryo vaccines) are widely used in developing countries because of their cost. These vaccines are banned in the US, Europe, and other countries because of potential severe side effects.
Vaccinated travelers are advised to delay the treatment for up to 1 day to receive CCV rather than DEV. Unvaccinated travelers don’t have this luxury, as the speed of receiving the vaccine is more important.
The immunoglobulin also comes in two forms. Derived from human and horse blood. Human rabies immunoglobulin (HRIg) is preferred, but it can be very expensive and even unavailable, especially outside of bigger cities.
The rabies vaccine is, therefore, a very economical and safe option for frequent travelers to Asia and Africa.
Long-term travelers, hikers, adventure travelers, travelers to remote areas, and children who are likely to pet dogs and less likely to report small bites and scratches will also benefit from the Rabies vaccination. It consists of 2 doses in 7 days.

Japanese Encephalitis vaccine
Japanese Encephalitis is a viral disease transmitted by a mosquito and it’s present only in Asia.
The transmission cycle includes pigs and rice fields and, therefore, occurs mostly in rural areas. The transmission is seasonal from April to November in northern parts of Asia, with a peak in July to September. In southeast Asia and India, the transmission depends more on local monsoon rain.
When infected, people have no symptoms at all in most cases. In less than 1 person out of 250, the nervous system is invaded, causing headaches, and in these patients ends in death in 5 – 30%. More than half of the survivors will have moderate to severe neurological problems.
Because of specific transmission, the overall risk for an average tourist is less than 1 in a million. Long-term travelers have a risk similar to the local population, which is 0.1 -1 in ten thousand per week.
Travelers spending more time in rural areas in Asia should consider the vaccination. Expats and travelers staying longer than a month will benefit from the vaccine protection.
However, because of the regional and seasonal character of this disease, the final recommendation should be provided after professional consultation at the travel clinic. Japanese encephalitis vaccine IXIARO® is applied in a two-dose regime. A booster dose is recommended one to two years later if the risk remains.
Dengue fever vaccine
There are an estimated 100 – 400 million dengue fever cases worldwide every year. The numbers are rising fast, more than tenfold compared to 20 years ago, as half of the world’s population lives in areas where Dengue fever transmission occurs.
The highest burden of this viral, mosquito-transmitted disease is in Asia, with around 70% of all cases. (This was different in past 2 years with Latin America leading the charts)
Although mostly asymptomatic or sometimes mild with symptoms like fever, headache, nausea, or rash, it can be severe and rarely fatal.
There are two relatively new vaccines available.
Dengvaxia® is a vaccine used in countries where it’s expected that a receiver has had contact with the dengue virus in their life.
Applying this vaccine to a dengue-naive (never infected) person creates a risk of a specific immune reaction, making the infection worse for the patient. Because of this, Dengvaxia vaccination is only available to previously infected people. This has to be confirmed by a blood test.
This vaccine is available in the US. However, it’s not recommended for travelers, but only for children 9 – 16 living in endemic areas like Puerto Rico, American Samoa, etc.
Qdenga® is the only vaccine approved for dengue-naive travelers or travelers in general. However, it’s only been approved by EMA (European Agency) since 2022.
The company behind the vaccine withdrew the application from the FDA and is therefore unavailable in the US. Another disadvantage is limited protection only to 2 serotypes (genetically different subtypes of the virus) out of 4.
Since not enough data are available on the Qdenga vaccine, it can only be recommended to any traveler with a previous Dengue infection who travels to an endemic country (a place where transmission occurs).
Swedish panel of experts says, it can be considered for not previously infected children 4-16 years old before a trip of any duration, or for adults traveling longer than 6 weeks in areas with high incidence (South East Asia).
In August 2024, the Swiss Expert Committee issued a recommendation against vaccinating anyone without a previous dengue infection.
It is still unknown if infection of vaccinated dengue-naive travelers by serotypes 3 and 4 could increase the risk of severe dengue fever. Therefore, the available recommendations are usually conservative.
Both vaccines have limited use in travelers. Even in a person previously traveling in Southeast Asia, if Dengue fever wasn’t confirmed while active or no symptoms were present, the positive laboratory results might not be enough to be sure that one has been infected by the virus.
With Sanofi-Pasteur planning to stop manufacturing Dengvaxia and Qdenga withdrawing its FDA application, we must wait for a better vaccine designed for travelers.
There is just one candidate in the late stage of clinical trials, with hopes of a safe and efficient vaccine against all four serotypes. It might be available in Brazil soon, as the local population experienced a huge Dengue outbreak in 2024. Then, it might be available for travelers, too.

Adolescents and young adults
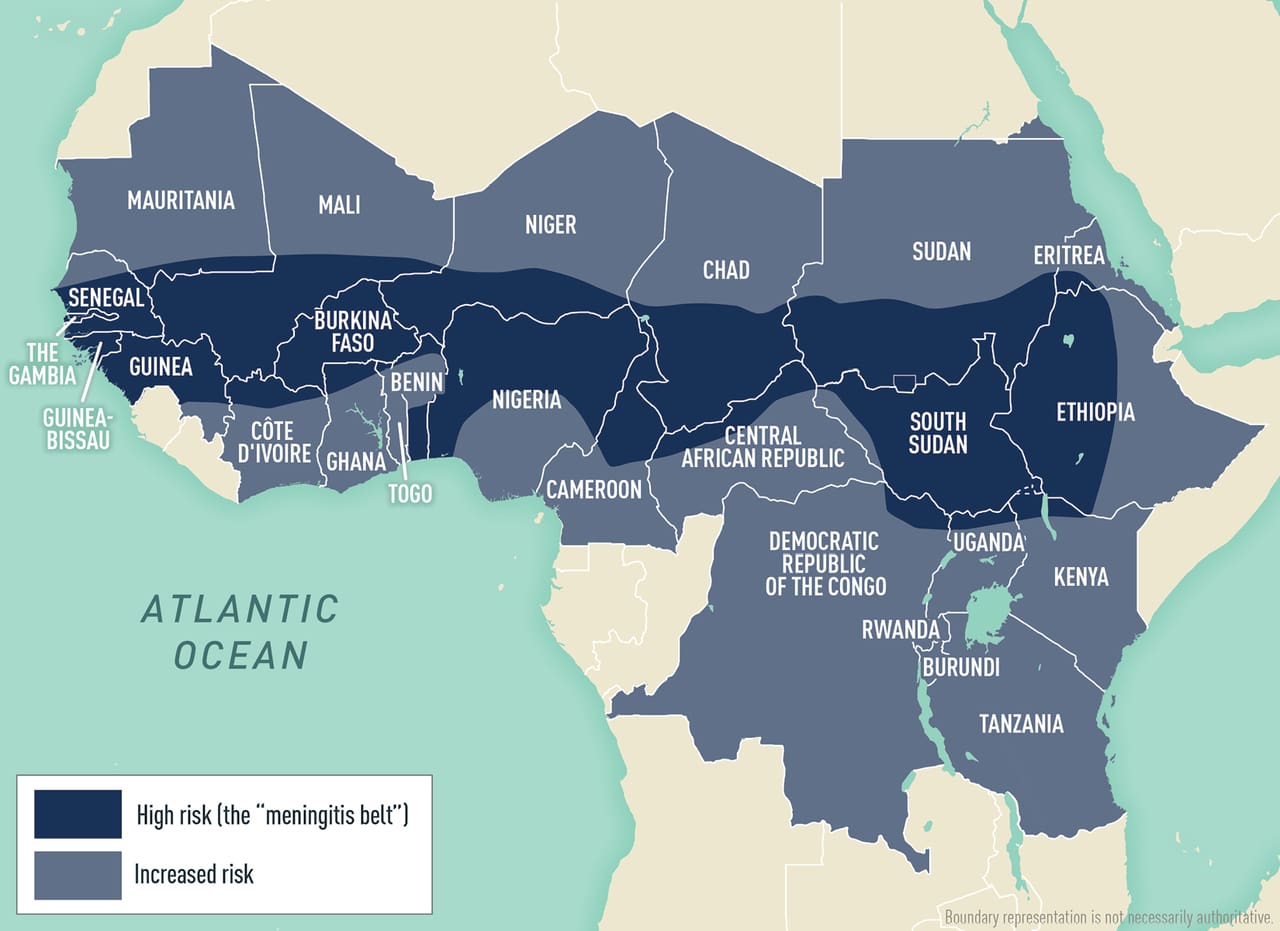
Menigococcal meningitis
Neisseria meningitidis is a bacteria present worldwide in up to 10% of hosts in the population. It’s transmitted through air from person to person, typically by kissing, sharing drinks or cigarettes, etc.
There are at least 13 subgroups of this pathogen, while the majority of meningococcal disease in developed countries is caused by type B, but type C is common too, especially in the US.
A higher chance of getting infected is in groups with a mix of diverse populations in crowded conditions. Typically young adults living in dormitories, attending concerts and parties a lot, especially with people from another countries can be at higher risk.
People enjoying nightlife activities, especially while traveling, for example, to the islands of Spain, etc, should consider vaccination against Meningococcal meningitis group B Bexsero® or Trumenba®.
Vaccination against serogroups A, C, W, and Y (in 1 vaccine) is recommended to all adolescents 11 – 12 years old by the CDC.
Vaccine against five most common serotypes PENBRAYA® has been recently approved by FDA.
HPV vaccine
Human papillomaviruses are distributed worldwide, with about 70% of all people contracting the virus at least once in a lifetime.
Some types of the virus can cause cervical cancer, and therefore, they’re recommended for girls 11 – 12 years old or 9 – 26 in some cases. Males aged 9 – 21 years are also recommended to be vaccinated in some countries to prevent transmission, genital warts, anal cancer and more.
The decline in cervical cancer cases in countries that implemented vaccination campaigns has been evident. Although travel probably doesn’t increase HPV risk, we include it in the list to not forget its importance.
Older travelers
These vaccines are not travel vaccines.
Pneumococcal vaccine is recommended for people older than 65, or adults younger but with various chronic illnesses.
Zoster (Shingles) vaccine Shingrix is recommended for most of the adults 50 years and older in the US.
Travelers to risk areas
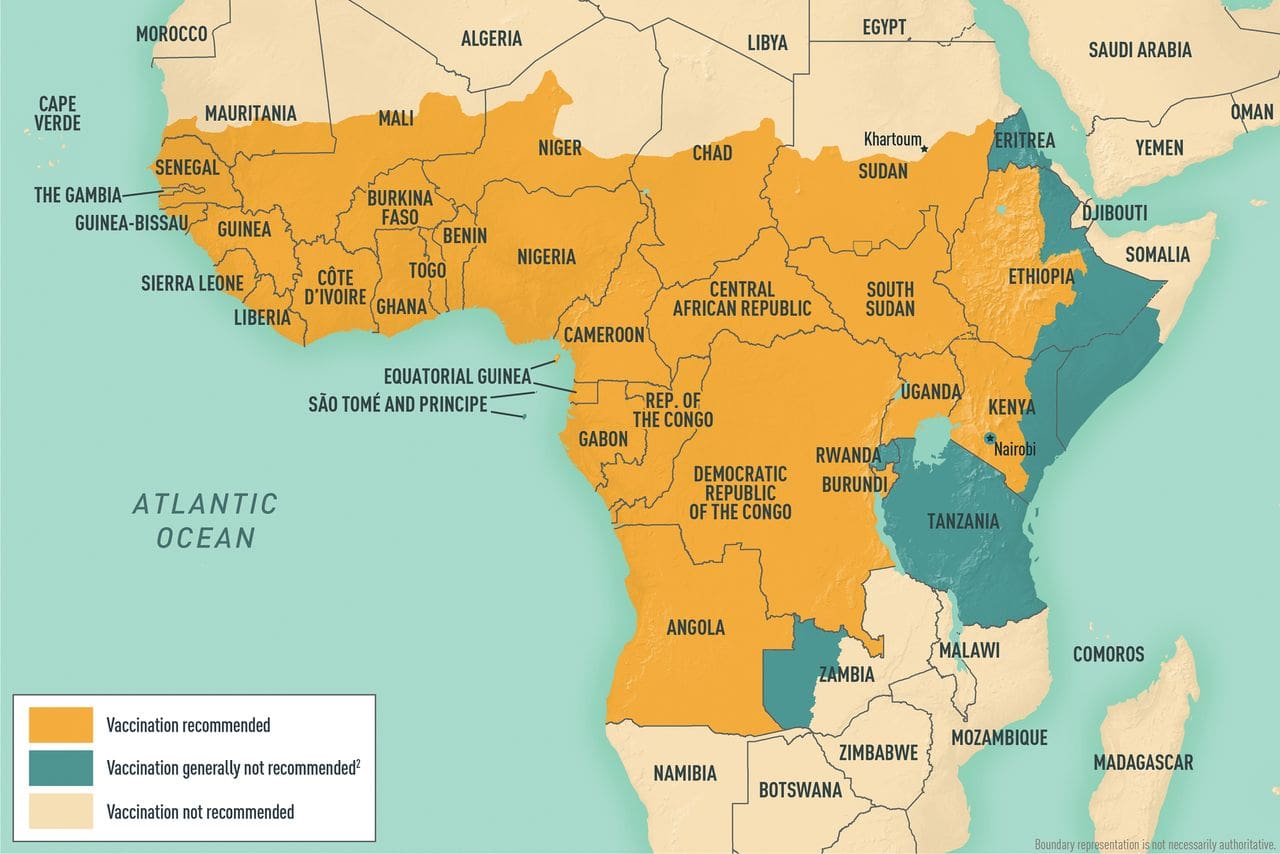
Yellow fever vaccine
Yellow fever transmission is limited to Subsaharan Africa and tropical parts of South America.
This virus is transmitted by a mosquito, and it presents with flu-like symptoms like fever, headache, nausea, etc. In 15% of cases, it can progress to severe disease that manifests with jaundice, bleeding, or organ failure and can end up with death in 25% – 50% of these patients.
Different transmission cycles exist, including infected primates in forested areas, but outbreaks in urban areas happen too, with humans as the main source and mosquitoes as a vector of infection. It’s often hard to assess the exact transmission areas as cases can be underreported in a ratio up to 1:250.
Transmission is seasonal, with peaks in July to October in Africa and January to March in South America.
The overall risk for infection and death is 10 times higher in West Africa compared to South America. However, reported yellow fever cases are usually in the low hundreds per year. In 2023, 476 cases were reported, 435 of which were on the African continent.
Even in countries with yellow fever transmission, especially in South America, the transmission is restricted to some areas. For example, places in high altitudes or urban areas usually pose no risk of getting yellow fever (this doesn’t apply to Africa, where urban outbreaks happen). That’s why consulting your itinerary with a specialist is needed to determine whether vaccination is recommended.
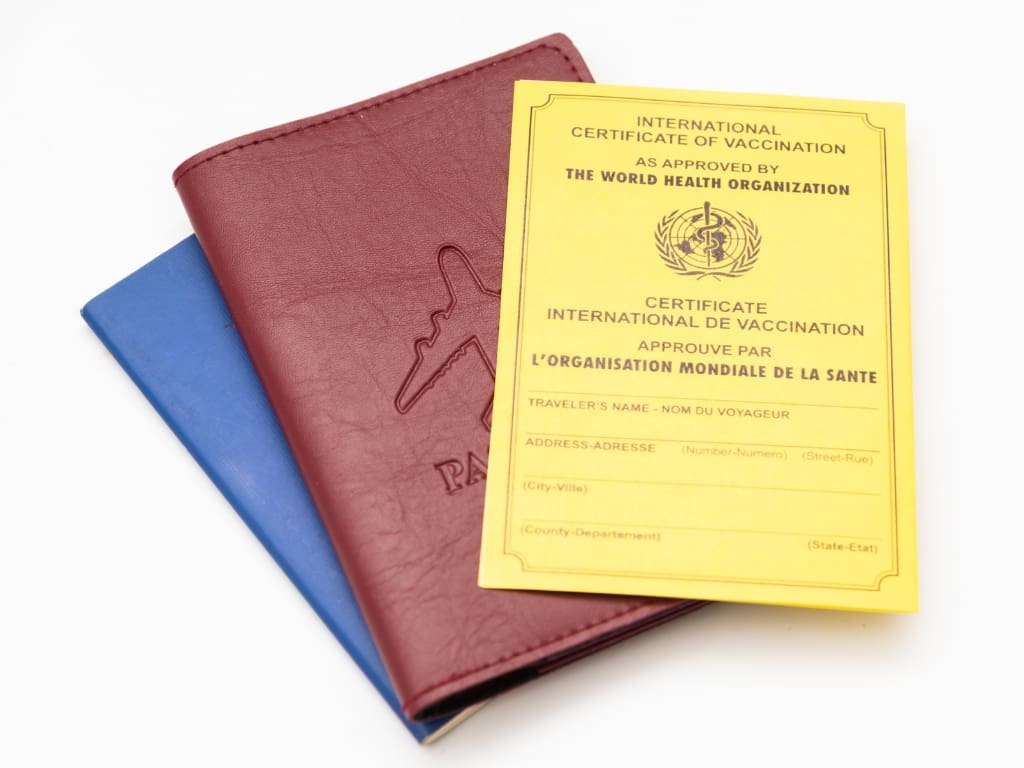
Yellow fever is the only disease for which proof of vaccination is mandatory to enter some countries.
Reason one is to protect the traveler entering a high-risk country.
Reason two is to protect the country’s population from the virus being imported by the traveler from the area where the transmission occurs. These countries typically have the right climate and environmental conditions to make Yellow fever transmission possible.
19 countries in Africa require proof of yellow fever vaccination from all travelers:
Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Congo, Côte d’Ivoire, Democratic Republic of the Congo, Gabon, Ghana, Guinea, Guinea-Bissau, Mali, Niger, Sierra Leone, South Sudan, Togo, Uganda.
In South America, only French Guiana has yellow fever vaccination as an entry requirement.
Many countries require proof of vaccination when a traveler arrives from a country with a risk of yellow fever transmission or transits for more than 12 hours (without leaving the airport transit zone).
According to WHO, 42 countries are currently at risk for transmission.
Current vaccination requirements by country can be found here.
List of Risk countries can be found here.
Yellow fever vaccination is only recommended for travelers to risky areas and countries that require proof of vaccination.
Extremely rare but severe adverse events, such as neurological disease and multiorgan failure, have been recorded.
These events occur in 0.2 to 0.8 cases per 100,000 doses, and the risk is greater in people older than 60. Many of those events occurred in patients with thymic disorder, and now administering the vaccine to these patients is contraindicated.
One dose should provide lifelong protection. Before 2016, a booster dose was required every ten years; now, a single dose is accepted for lifetime protection even in people vaccinated before this year.
After administering the vaccine in a certified vaccination center, the stamp in the International Certificate of Vaccination or Prophylaxis (ICVP or “yellow card”) should be accepted worldwide.
Any medical contraindication to vaccination must be correctly written in the ICVP with the reason explained and signed by a physician. Entry to countries requiring proof of vaccination should be allowed in such cases, but it always depends on border control and can be declined. Contacting the country’s embassy before departure might be necessary to ensure smooth entry to the country.
List of certified YF vaccination centers in the USA can be found here.
What if I’m not vaccinated against yellow fever or if I don’t have a medical waiver?
Border control will either deny you entry, mandate quarantine for up to 6 days or give you a chance to be vaccinated at the airport.
Meningococcal vaccine
Yes menigoccoccal menigitis again!
Vaccination against serogroups A, C, Y, and W-135 is required for pilgrims on the hajj and umrah in Saudi Arabia.
The same vaccine is also recommended for travelers visiting countries in the so-called meningitis belt (a belt-shaped area of equatorial Africa) during the dry season from December to June and for all long-term travelers or travelers staying with the local population.
Vaccines like Menveo® and MenQadfi® in the US plus Nimenrix® in Europe are widely used and effective in preventing potentially invasive disease. Single dose application with booster every 3 – 5 years is recommended.
Polio vaccine
The Polio vaccine is administered worldwide as a routine vaccination of children to prevent this crippling disease. Hopefully, it will soon be the second disease ever eradicated.
Wild polio currently circulates only in a few countries, and in 2023, there were just 12 cases recorded by WHO in Afghanistan and Pakistan.
We might be close to eradication and the risk for travelers even to countries with reported cases is extremely low, but still, importing the virus from these countries could have catastrophic consequences.
That’s why other than routine vaccination of children, even fully vaccinated adults may be advised to recieve a booster dose if they are at risk of exposure to poliovirus.
Tickborne encephalitis vaccine
Tickborne encephalitis is the most common central nervous system infection in many central and Northern European countries. Around 1% of the cases are deadly for the European subtype and up to 20% for the Far Eastern subtype. Almost half of the patients with encephalitis will not fully recover.
Travelers are at risk when doing outdoor activities in forested areas where infected ticks are present. Campers, hikers, or outdoor workers in these areas from April to November should consider a 3-dose vaccination with TICOVAC® in the US or FSME-IMMUN® in Europe.

Traveling to areas with active outbreak
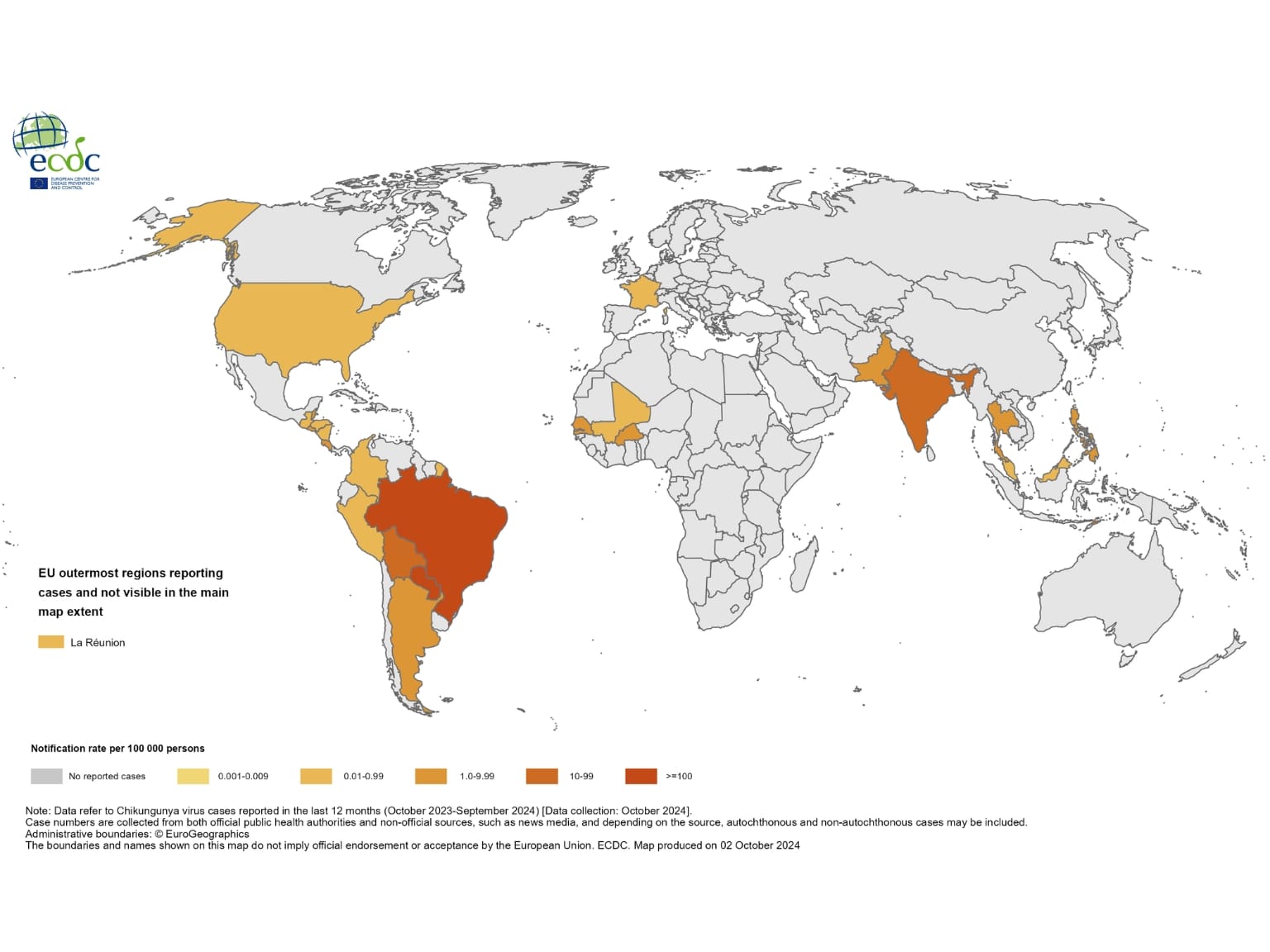
Chikungunya vaccine
The Chikungunya vaccine has been approved for travelers in the US since February 2024.
The recommendations are very straightforward and apply to travelers to areas with active outbreaks.
At the time of writing this article, there are no outbreaks. The last large outbreak was in Chad in 2020.
Update: As of February 2025, there is an outbreak of chikungunya in the states of Maharashtra and Telangana, India.
Travelers that might consider vaccination include people 65 years and older or long-term travelers (6+ months) to countries with reported cases of this viral, mosquito-transmitted disease. The list is provided by the CDC.
Mpox vaccine
Mpox, also known as Monkeypox, received attention in 2024 as there was an outbreak of the viral disease in Central and Eastern Africa. There is an ongoing human transmission, mostly in the Democratic Republic of Congo (DRC), which occurs through bodily fluids or contact with skin affections.
JYNNEOS® vaccine was originally developed to be used in the event of a smallpox bioterrorist attack. However, because of its safety profile and efficacy against Mpox, it was authorized for emergency use by the FDA in 2022.
This two-dose vaccine is currently recommended for people anticipating sexual activities with new partners in countries with ongoing human-to-human Mpox transmission.
Healthcare and relief workers
Cholera vaccine
As I said in the beginning, the presence of the infection isn’t necessarily an indication for vaccination. For tourists traveling to countries even with cholera outbreaks, the risk remains low.
This vaccine is primarily for emergency workers getting in a close contact with people in epidemic areas, typically refugee camps, slums, or after a natural disaster.
Oral cholera vaccine Dukoral® has some crossreactivity with a subtype of E.coli responsible for most cases of traveler’s diarrhea and, therefore, is approved and marketed for this indication to travelers. However, the overall effect on lowering the probability of traveler’s diarrhea isn’t great or long-lasting.
Tuberculosis - BCG vaccine
The most recent WHO recommendation is to vaccinate newborns or early infants with BCG vaccine in countries with a high prevalence of Tuberculosis.
Because of its variable efficacy in adults, vaccination is not recommended for travelers to these regions, and the BCG vaccine is not available in the US.
Some experts recommend vaccinating adult healthcare workers planning to work in countries with a high burden of drug-resistant Tuberculosis.
Final words
The recommendations for children, pregnant women, immunocompromised people, and other specific groups were not included because of the variability that needs a personalized approach.
As you may have read, many vaccine-preventable diseases have specific transmission methods, areas, environmental factors, seasons, etc.
That’s why every traveler, especially first-time travelers to tropical destinations, should consult a travel health expert to assess and plan appropriate vaccinations for the upcoming trip and beyond.
Resources
Centers for Disease Control and Prevention (CDC), and Jeffrey B. Nemhauser, CDC Yellow Book 2024: Health Information for International Travel (New York, 2023; online edn, Oxford Academic, 23 Mar. 2023), https://doi.org/10.1093/oso/9780197570944.001.0001
Travel Medicine, 4th Edition – December 13, 2018, Authors: Jay S. Keystone, Phyllis E. Kozarsky, Bradley A. Connor, Hans D. Nothdurft, Marc Mendelson, Karin Leder, Language: English, Hardback ISBN: 9780323546966
Jackson, B. R., Iqbal, S., Mahon, B., & Centers for Disease Control and Prevention (CDC) (2015). Updated recommendations for the use of typhoid vaccine–Advisory Committee on Immunization Practices, United States, 2015. MMWR. Morbidity and mortality weekly report, 64(11), 305–308.
Martin Angelin, Jan Sjölin, Fredrik Kahn, Anna Ljunghill Hedberg, Anja Rosdahl, Paul Skorup, Simon Werner, Susanne Woxenius, Helena H. Askling, Qdenga® – A promising dengue fever vaccine; can it be recommended to non-immune travelers?, Travel Medicine and Infectious Disease, Volume 54, 2023, 102598, ISSN 1477-8939, https://doi.org/10.1016/j.tmaid.2023.102598
Menon, S., Wilder-Smith, A. New Vaccines on the Immediate Horizon for Travelers: Chikungunya and Dengue Vaccines. Curr Infect Dis Rep 25, 211–224 (2023). https://doi.org/10.1007/s11908-023-00811-x.
Vianney Tricou, Delia Yu, Humberto Reynales, Shibadas Biswal, Xavier Saez-Llorens, Chukiat Sirivichayakul, et al., Long-term efficacy and safety of a tetravalent dengue vaccine (TAK-003): 4·5-year results from a phase 3, randomised, double-blind, placebo-controlled trial, The Lancet Global Health, Volume 12, Issue 2, 2024, Pages e257-e270, ISSN 2214-109X, https://doi.org/10.1016/S2214-109X(23)00522-3.
Gautret, P., & Parola, P. (2014). Rabies in travelers. Current infectious disease reports, 16(3), 394. https://doi.org/10.1007/s11908-014-0394-0
David O Freedman, A new dengue vaccine (TAK-003) now WHO recommended in endemic areas; what about travellers?, Journal of Travel Medicine, Volume 30, Issue 7, October 2023, taad132, https://doi.org/10.1093/jtm/taad132
Eperon, G., Veit, O., Antonini, P., Fehr, J., Haller, S., Hatz, C., Landry, P., Neumayr, A., Niederer-Lohrer, A., Schlagenhauf, P., de Vallière, S., Staehelin, C., & on behalf of the Swiss Expert Committee on Travel Medicine (ECTM). (2024). Vaccination against dengue fever for travellers: Statement of the Swiss Expert Committee for Travel Medicine, an organ of the Swiss Society for Tropical and Travel Medicine, August 2024. Swiss Medical Weekly, 154(9), 3858 . https://doi.org/10.57187/s.3858
Mary-Claire R Walsh, Mohammed Shafiul Alam, Kristen K Pierce, Marya Carmolli, Masud Alam, Dorothy M Dickson, Dan M Bak, Sajia Afreen, Forida Nazib, Kibria Golam, Firdausi Qadri, Sean A Diehl, Anna P Durbin, Stephen S Whitehead, Rashidul Haque, Beth D Kirkpatrick, Safety and durable immunogenicity of the TV005 tetravalent dengue vaccine, across serotypes and age groups, in dengue-endemic Bangladesh: a randomised, controlled trial, The Lancet Infectious Diseases, Volume 24, Issue 2, 2024, Pages 150-160, ISSN 1473-3099, https://doi.org/10.1016/S1473-3099(23)00520-0.
Stanaway, Jeffrey D et al., The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017, The Lancet Infectious Diseases, Volume 19, Issue 4, 369 – 381 https://doi.org/10.1016/S1473-3099(18)30685-6
https://www.cdc.gov/chikungunya/hcp/vaccine/index.html
https://www.cdc.gov/meningococcal/hcp/vaccine-recommendations/index.html
https://www.cdc.gov/mmwr/volumes/72/wr/mm7249a3.htm
https://wwwnc.cdc.gov/travel/notices/level2/clade-1-mpox-central-eastern-africa
https://travelhealthpro.org.uk/factsheet/20/rabies
https://www.who.int/news-room/fact-sheets/detail/yellow-fever
Disclaimer:
The information provided in this blog post is for general informational and educational purposes only and is not a substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any health problem. The use or reliance on any information provided in this blog post is solely at your own risk.